SSZT821 January 2018 BQ25100 , BQ25120A
As healthcare coverage expands to cover emerging technologies, batteries shrink and interconnectivity improves, the medical field is close to a paradigm shift in treatment options. In the next decade, doctors may commonly monitor hundreds of patients using online tools, avoiding in-person medical checkups and allowing health care systems to cope with an increasing volume of patients.
Following this trend, more and more medical and personal electronics companies are embracing wearables to improve patient outcomes and higher quality of service during both the in- and outpatient treatment stages. These companies are helping increase patients’ quality of service through a variety of innovations to medical equipment, but one of their main focuses is to modify designs so that all patient care equipment is capable of following a patient throughout their stay. Currently, significant resources are dedicated to moving a patient and exchanging monitoring equipment between different wards. Nurses have to prepare large equipment to receive a patient from other wards, and logistics must be coordinated to return equipment to their original locations after a patient transfer, all of which costs time and effort. Equipment with better mobility smooths the transition from the intensive care unit, to the general ward to a patient’s eventual release. By eliminating the need to coordinate between departments or even outside organizations the transition-of-care process becomes more convenient by allowing the equipment to stay with the patient.
Portability is not a new idea, since most traditional medical equipment has batteries already (albeit extremely large ones). The size of these batteries has made it too challenging for most patients to be easily mobile. In an effort to resolve this problem, companies have taken a new approach, using basic sensors as the primary monitoring tools and delegating auxiliary functions through connections to medical networks. Offloading all processing, storage and other non-monitoring processes reduces the cost of and surface area of medical equipment, making medical devices less expensive, lighter and more versatile. By monitoring patient information like those shown in Figure 1, medical devices from cutting-edge wearables to traditional hospital equipment like bedside monitors, drug-infusion pumps and sensor-packed beds can help patients and their providers stay connected.
 Figure 1 Patient Information That Can
Be Tracked and Transmitted by Wearable Monitors
Figure 1 Patient Information That Can
Be Tracked and Transmitted by Wearable MonitorsInterconnectivity improves a multitude of routine medical processes, including documentation, asset tracking and patient care. Automated documentation prevents mistakes when recording vitals. Constantly connected equipment maximizes use and makes it possible for machines to facilitate or even completely accomplish routine medical procedures.
Take for example the process of preventing bedsores on bedridden patient. Traditionally, a nurse has to remember to change and record the patient’s position every few hours to prevent pressure sores. But a connected hospital bed or a sensor worn by the patient can expedite this process, automatically tracking movement and alerting nurses when action is necessary. These devices would also create an accurate log of the patient’s different positions, giving doctors a useful resource if the patient reports any pain or change in status.
Through small improvements like these, a revolution is brewing. Doctors are now doing more with less, but only as long as these devices remain on. For this exact reason, all-day battery life is essential for patient convenience and outcomes.
| Want reference designs for wearable fitness & activity monitor applications? | |

|
Check out these four battery-management reference designs for your next energy storage subsystem |
Constant communication and other features like touch screens consume energy at levels that prevent disposable batteries from being a viable solution within this new monitoring space. These batteries would drain quickly by providing this power, adding a large cost to the operation of each device. Meanwhile rechargeable lithium-ion batteries are powerful enough to resolve the power problem but they require much more consistent temperature and protection, and charging them correctly is a big concern. For medical applications that are small and susceptible to electrical noise linear chargers can be used for the charging task. Linear chargers are simple to design into any power block and can provide charge currents of up to 1.5A, with smaller solution sizes than their switching counterparts.
TI’s smallest linear charger, the bq25100, has termination current control with precision down to 1mA, a leakage current of only 75nA (which is negligible compared to the self-discharge rate of the battery cell) and one of the lowest bill-of-materials (BOM) costs on the market. This makes the bq25100 ideal for simple applications that require less than 250mA of charge current or precise termination currents, such as wearable applications and patient monitors.
If you need a more complex charger, the bq25120A is a great alternative. This charger comes with integrated I2C, push-button controls, a low-dropout regulator (LDO), a buck converter, and fast charging and power-path capabilities, while still being smaller than three grains of rice. It has the capability to power systems while simultaneously charging the battery, allowing for instant-on functionality. The push-button control facilitates interfacing with the microcontroller (MCU) over the rails or interrupts, allowing easy access to different modes of operation. Fast charging allows for a high amount of charge in a small period of time in exchange for some extra wear and tear on the battery.
The inclusion of I2C communication control adds a whole world of customization to this device. For example, the I2C interface enables you to customize the charge profile through the MCU. You can configure the charge voltage, charge current, termination threshold, input current limit, safety timer limit and much more to meet a wide range of specifications. This customization results in light wearable solutions with small batteries to charge without having to sacrifice performance or customization. Customization also enables lower termination currents, which means you can charge batteries to higher capacities every cycle. See Figure 2.
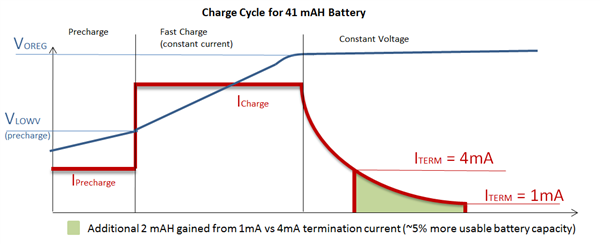 Figure 2 The Benefits of a Low
Termination Current
Figure 2 The Benefits of a Low
Termination CurrentFigure 3 shows the use of either the bq25100 or bq25120A linear charger in a wearable electrocardiogram (ECG) patch. This ECG patch would enable someone who has had a recent heart procedure to constantly track their vitals without having embarrassing wires or machines connected to them. The miniaturization of devices like the bq25120A makes this design possible.
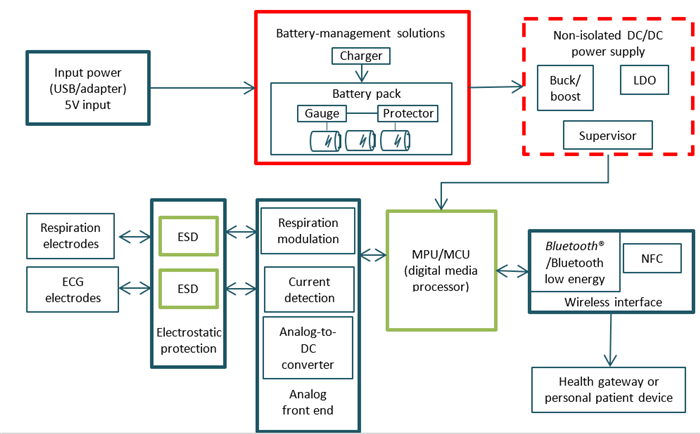 Figure 3 ECG Patch System
Diagram
Figure 3 ECG Patch System
DiagramBatteries are becoming an integral part of medical technology because of the growing need for small solution size, which enables portability, longevity and continuous interconnectivity. Using devices that constantly monitor the state of a patient’s health not only enhances patient care, but improves healthcare processes within a hospital or medical facility. Size-conscious linear charges like the bq25100 and bq25120A maximize the longevity of the battery, allowing something like an ECG patch to keep up with the patient’s health needs without the constant battery replacement that would interfere with monitoring.
Of course, TI offers many more linear chargers than just the ones I’ve mentioned here, and we are continually developing more variations to keep up with the latest demands from the medical industry. This includes supporting the newest waves of patient monitoring systems that will help impact modern health care from the ICU to a patient’s home for the better by making patients more mobile and providers more efficient. The future is uncertain, but it does look bright.
Additional resources:
- Explore TI’s portfolio of intelligent, compact linear chargers.
- View reference designs for wearable fitness monitors and other medical devices.
- Buy the bq25100 evaluation module or the bq25120A EVM.
- Watch this video on charging considerations for different battery chemistries for portable medical applications.
- Read a blog on what’s next for medical ultrasound.